Orthopedic medical devices live in a high-stakes environment. Whether it’s hip and knee joint replacements, bone fixators, modular trays, or surgical instruments, surgeons expect every sterile pack to open cleanly, present the device in the correct orientation, and maintain a reliable sterile barrier from production through to the operating room.
For orthopedic device companies, sterile packaging is just as important as product design. It links orthopedic device manufacturing, sterilization methods, supply chain management, and regulatory preparation into one connected system. When this system works, surgical teams can focus on patient care instead of worrying about packaging failures, tamper-evident designs, or recalled processes.
This article explores how sterile packaging for orthopedic devices supports safety, performance, and regulatory compliance—while also creating practical benefits for operations and inventory management.
Why Sterile Packaging Matters in the Orthopedic Industry
Sterile packaging for orthopedic devices must do more than simply cover a product. It has to create and maintain a sterile barrier that protects medical instruments, surgical implant devices, and finished orthopedic devices against contamination throughout the entire lifecycle. The goal is to maintain sterility “until the point of use or expiration date,” making packaging performance directly linked to patient safety.
In the orthopedic industry, packaging is expected to:
- Protect against microbial ingress and physical damage.
- Support validated sterilization processes.
- Withstand distribution conditions defined in standards such as ASTM D4169.
- Integrate with hospital workflows so surgical teams can handle orthopedic systems quickly and confidently.
The same sterile packaging for orthopedic industry applications must work consistently whether the device is a single orthopaedic implant, a combination product with accessories and digital healthcare products, or a full orthopedic system with multiple instruments in modular trays.
Because these expectations are high, orthopedic packaging solutions must be engineered from the start—not treated as an afterthought toward the end of product development.
Regulatory Framework: ISO 11607, ISO 13485, and GMP Standards
Regulators view packaging as part of the medical device, and that means the packaging process, packaging validation, and packaging components all sit within a broader quality and infrastructure framework.
Key elements include:
- ISO 13485: Quality management systems for the medical device industry, including contract manufacturing and contract packing services.
- ISO 11607: The global reference for sterile barrier packaging systems, covering design, materials, validation testing, and forming a Sterile Barrier System with a protective packaging system.
- GMP standards: Good manufacturing practice defines how clean room packaging, sterilisation processes, and documentation should be controlled.
Orthopedic device companies depend on partners who understand how these standards link together. For example, an ISO 13485 certified partner can help align packaging development and packaging validation with the overall validation process of finished orthopedic devices, including sterilization methods, shelf life, and labeling requirements such as Unique Device Identification (UDI) labels.
When packaging is designed with regulatory requirements in mind, the submission process runs more smoothly. Packaging validation reports, simulated distribution data, and sterile barrier protection evidence become part of a cohesive regulatory preparation package instead of a reactive scramble.
Design for Manufacturing: Connecting Product and Packaging
For orthopedic systems, packaging cannot be separated from product design and product development. Design for Manufacturing (DFM) should extend beyond the implant’s geometry and machining steps to include the packaging format and the packaging process.
Examples of integrated DFM thinking:
- Choosing medical-grade materials compatible with the appropriate sterilization method, typically gamma radiation or ethylene oxide.
- Selecting blister packaging or pouches sized for efficient line speeds and ergonomic opening by surgical teams.
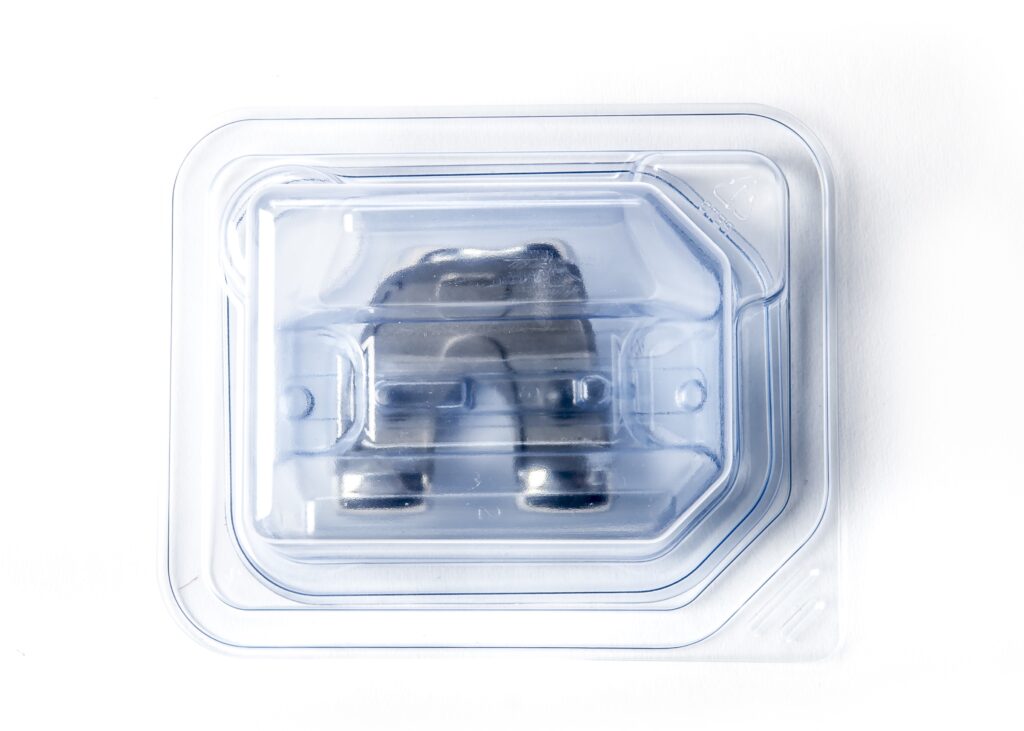
- Engineering compression-molded trays or foam packaging solutions that stabilize an orthopaedic implant while still presenting it clearly in the sterile field.
- Coordinating modular trays, color-coded seals, and labels so surgical instruments are easy to identify at a glance.
Early collaboration between device engineering, packaging innovation teams, and contract manufacturing partners leads to a custom solution that supports both clinical use and manufacturability. This approach helps avoid late-stage changes that can trigger repeated validation testing, repackaging, or even recalled processes if risks are not properly addressed.
Materials, Formats, and Sterile Barrier Protection
Orthopedic medical devices place unique demands on packaging materials. The packaging must resist puncture from sharp devices, protect heavy components like orthopedic implant systems, and stand up to sterilization and shipping.
Common material considerations include:
- High-density polyethylene (HDPE) and other robust plastics for rigid or semi-rigid trays.
- Film and Tyvek® structures that maintain microbial barrier performance through gamma or EtO sterilization.
- Paperboards and inserts that meet cleanliness expectations and support user-driven healthcare information, such as IFUs or digital healthcare products via QR codes.
Packaging formats often used for orthopedic devices:
- Blister packaging with a pre-validated seal.
- Pouches designed as a Sterile Barrier System with outer protective bags.
- Rigid trays with sterile barrier lids and modular trays inside for surgical instruments and medical instruments.
By combining these elements, sterile barrier packaging systems create both impact and protection. Correctly specified seal widths, validated sealing parameters, and tamper-evident designs give teams confidence that the microbial barrier has been preserved from sealing through to opening in the OR.
Cleanroom Operations, Sterilization, and Contract Packing Services
For orthopedic device companies, outsourcing to a partner with ISO 7 & 8 cleanrooms and robust sterilization services can simplify the path from components to finished orthopedic devices.
A typical sequence for clean room packaging and sterilisation processes might include:
- Component receipt and inspection – Packaging components and orthopedic device components arrive and are verified against specifications.
- Assembly and packaging – Devices are assembled (when applicable) and packaged inside ISO 7 & 8 cleanrooms using pre-validated packaging or custom packaging designs.
- Sterilization methods – Batches are processed using gamma radiation or EtO sterilization, whichever is appropriate for the device and materials.
- Release and distribution – After meeting bioburden, sterility, and packaging integrity requirements, the product is released into supply chain management and inventory management systems.
By integrating contract packing services with sterilization and quality assurance, orthopedic device manufacturing teams can consolidate vendors and minimize handoffs.
Partners like PRO-TECH Design can manage the interfaces between packaging development, sterilization methods, and logistics, reducing complexity while maintaining compliance. This approach reflects how many orthopedic manufacturers are shifting toward integrated service partners who can support both day-to-day production needs and long-term program stability.
Packaging Validation, Shelf Life, and Risk Reduction
A strong validation process protects both patients and brands. For orthopedic devices, packaging validation and validation testing typically address:
- Seal strength and integrity – Confirms that the pre-validated seal or sealed sterile barrier maintains protection over time.
- Microbial barrier performance – Verifies that the sterile barrier prevents microbial ingress under defined conditions.
- Aging and shelf life – Uses accelerated or real-time studies to determine how long sterile barrier protection and material performance remain acceptable.
- Distribution simulation – Uses protocols such as ASTM D4169 to test how packaging performs under transport shocks, vibrations, and compression.
Thorough validation ties test data to risk management files and regulatory requirements. When done well, it supports long shelf life targets and helps avoid complaints, field returns, or corrections related to packaging failures.
Operational Benefits: Surgical Efficiency and Supply Chain Performance
Sterile packaging is also a powerful operational lever. Thoughtful orthopedic packaging solutions contribute directly to surgical efficiency, hospital workflows, and the wider supply chain.
Examples include:
- Color-coded seals and UDI labels that allow quick identification of hip and knee joint replacements, bone fixators, and other orthopaedic implant families.
- Modular trays that organize instruments in the order needed for the procedure, supporting surgical efficiency and reducing search time in the sterile field.
- Pack counts and box quantities tuned to supply chain management needs, reducing partial shipments and stockouts.
- Tamper-evident designs that simplify receiving inspections and help detect shipping damage.
Over time, small improvements in packaging and labeling can lead to measurable time savings in the OR and fewer disruptions across distribution networks.
Sustainability, Local Suppliers, and Packaging Innovation
Orthopedic device companies are under growing pressure to reduce their carbon footprint while maintaining high levels of protection. Packaging innovation plays a central role in this balance.
Practical strategies include:
- Working with local suppliers for packaging components to shorten transport distances and increase agility.
- Reducing excess materials through careful product design and packaging development
- Exploring additive manufacturing and other technologies for rapid prototyping of trays, dunnage, and custom solution components.
- Using data from supply chain management and inventory management systems to fine-tune packaging sizes and formats.
Specialized suppliers are also there to contribute specialized foam packaging solutions, compression-molded components, and high-performance inserts that stabilize devices while minimizing waste. Done thoughtfully, sustainability initiatives can support user-driven healthcare goals by minimizing clutter in the OR and reducing the number of items that need to be managed, stored, or discarded.
Digital Technologies and Artificial Intelligence in Packaging
The medical device industry is increasingly exploring how digital tools and artificial intelligence can support packaging operations. While packaging will always be a physical discipline, data-driven systems can improve:
- Forecasting for packaging components and raw materials.
- Traceability for Sterile Barrier System lots, sterilization records, and UDI labels.
- Monitoring of sealing equipment, sterilization processes, and cleanroom conditions.
In Research and Development, digital twins and simulation tools can evaluate design concepts for new orthopedic packaging solutions before committing to tooling. Combined with strong human expertise on the shop floor, these tools help orthopaedic implant and orthopedic systems teams iterate faster while maintaining compliance.
Turning Orthopedic Packaging into a Strategic Advantage
A well-thought-out packaging strategy also becomes a strategic conversation about where orthopedic companies want to go next. As portfolios expand, indications grow more complex, and health systems demand both reliability and value, the packaging decisions made today will either support that growth or constrain it.
Teams that treat packaging as an integrated design, quality, and operations discipline are better positioned to respond quickly to new indications, new materials, and evolving regulatory expectations.
For many organizations, that shift happens when packaging, manufacturing, quality, and supply chain stop working in silos and begin building shared roadmaps. Questions like “How will this tray respond to the sterilization method we’re using?” or “What happens to OR workflow if we change counts or labels?” start to be asked at the concept stage, not at the validation deadline. That mindset reduces friction later on and gives commercial and clinical leaders more confidence when planning launches or line extensions.
How PRO-TECH Design Supports Orthopedic Device Companies
Partners such as PRO-TECH Design bring practical experience from running ISO 7 cleanrooms, coordinating sterilization, and supporting orthopedic programs over multiple product generations.
Support often includes:
- Early-stage consultations on product development, packaging innovation, and design for manufacturing.
- Transition from lab builds to controlled production environments, including ISO 7 cleanrooms and GMP standards.
- Selection and qualification of medical-grade materials and packaging components—trays, lids, pouches, labels, and protective elements.
- Coordination of validation testing, including packaging validation, sterilization validation, and shelf life studies.
- Ongoing packaging process monitoring and continuous improvement to align with quality and infrastructure objectives.
So, whether you are launching a new orthopedic implant platform, updating packaging for an existing combination product, or consolidating vendors to simplify orthopedic device manufacturing, PRO-TECH Design can operate as an extension of your internal team—linking packaging requirements, regulatory expectations, and day-to-day production realities.
If you’d like to explore what this could look like for your line of orthopedic devices, connect with our team to review your current packaging approach, identify risks and opportunities, and outline a practical path to more robust, scalable sterile packaging systems.
FAQs
- What makes sterile packaging for orthopedic devices different from other device categories?
Orthopedic devices often involve heavy components, sharp edges, and complex orthopedic systems with multiple instruments and implants. Packaging must provide sterile barrier protection while also resisting punctures and shocks during shipping. Designs frequently include rigid or semi-rigid trays, blister packaging, or double-pouch formats that balance protection, usability, and sterilization process compatibility.
- How does ISO 11607 relate to orthopedic packaging solutions?
ISO 11607 defines requirements for sterile barrier packaging systems, from material selection and design to validation testing and documentation. For orthopedic packaging solutions, it guides how trays, lids, pouches, and seals are designed and tested to maintain a Sterile Barrier System through sterilization, distribution, and storage until use in the operating room.
- What sterilization methods are commonly used for orthopedic medical devices?
Gamma radiation is the most common method because of its effectiveness on metal and certain polymers commonly found in orthopedic devices. It also penetrates dense devices and causes minimal temperature change. Ethylene oxide (EtO sterilization) is the second most common sterilization method used. The choice depends on device materials, complexity, and compatibility with medical-grade materials and packaging components. Packaging engineers work closely with sterilization services and quality teams to confirm that seals, materials, and labeling perform well under the selected sterilization processes.
- Why is packaging validation so important for orthopedic devices?
Packaging validation and the broader validation process confirm that the sterile barrier, microbial barrier, and overall packaging system perform as intended over the product’s shelf life and distribution routes. Validation testing, including seal strength, integrity, aging, and distribution simulation, supports regulatory requirements and helps prevent damage, contamination, and recall processes.
- How do packaging choices affect surgical efficiency?
Well-designed orthopedic packaging can improve surgical efficiency by presenting devices in a logical order, using modular trays, color-coded seals, and clear labeling. This helps surgical teams identify the correct orthopaedic implant, surgical instruments, and medical instruments quickly, reducing time spent searching for components and allowing the team to focus on the procedure.
- What role do contract manufacturing partners play in orthopedic packaging?
Contract manufacturing and contract packing services providers with ISO 13485 certification and ISO 7 certified cleanrooms can manage assembly, packaging, sterilization services, and inventory management under one quality system. This helps orthopedic device companies streamline supply chain management, maintain GMP standards, and align packaging development with long-term production needs.
- Can pre-validated packaging help speed time to market?
Yes. Leveraging pre-validated packaging, such as standard tray and lid systems with known performance, can shorten development and validation timelines. These systems may already have established data for seal performance, distribution testing, and compatibility with common sterilization methods, which can then be supplemented with product-specific studies for finished orthopedic devices.

