In the healthcare industry, maintaining the highest level of cleanliness and sterility is not just a recommended practice, it’s an absolute necessity. For medical devices that come into direct contact with patients, their sterility directly impacts patient safety and treatment effectiveness.
In this article, we will explore the significance of sterile packaging, various methods used, sterilization techniques employed, packaging validation, and more.
By examining these aspects, we can gain a deeper understanding of how sterile packaging safeguards patients and facilitates optimal healthcare outcomes.
What is Sterile Packaging for Medical Devices
Sterile packaging for medical devices is a specialized niche that involves the use of specific materials, techniques, and protocols to create a barrier that ensures the sterility and integrity of the devices. It serves as a critical line of defense in preventing healthcare-associated infections (HAI), complications, and adverse events in patients. According to the Centers for Disease Control and Prevention (CDC), HAIs affect approximately 1 of every 31 hospitalized patients at any given time in the U.S. alone, underlining the importance of sterile packaging in combating these infections.
The sterile packaging process begins with the careful selection of appropriate materials. These typically include polyethylene, polypropylene, and Tyvek®, which is a high-density polyethylene nonwoven material known for its excellent microbial barrier properties. These materials are chosen due to their ability to provide a reliable barrier and the subsequent sterilization techniques employed depend on various factors such as the device’s material, complexity, and heat sensitivity.
Once sterilized, the packaging undergoes a rigorous validation process followed by quality control measures, implemented to monitor and maintain the highest standards of cleanliness and sterility throughout the packaging process.
According to the Food and Drug Administration (FDA), medical device packaging must prevent microbial ingress, protect the device from damage, and provide an unambiguous method of presentation at the point of use.
Why is Sterile Packaging for Medical Devices Important?
Patient Safety
The primary goal of sterile packaging is to protect patients. Without it, medical devices could become contaminated with bacteria, viruses, or other harmful substances, leading to infections or complications during treatment.
Surgeons and healthcare professionals clearly rely on sterile instruments and devices. But patient safety extends beyond the healthcare setting, as medical devices may be used in home care or other non-clinical environments. In these circumstances, sterile packaging ensures that these devices reach patients in a sterile condition, minimizing the risk of infections or complications that could arise from improper handling or storage.
Compliance with Regulations
Medical device manufacturers must adhere to strict regulations and guidelines set forth by regulatory authorities. These regulations, such as the FDA’s Current Good Manufacturing Practices (cGMP) and the ISO 13485 standard, emphasize the importance of sterile packaging.
Compliance with these standards is not only a legal requirement but also a means to ensure the safety and efficacy of medical devices. By implementing proper sterile packaging practices, manufacturers can meet regulatory requirements, obtain necessary certifications, and demonstrate their commitment to delivering high-quality and safe medical devices.
Protection against Contamination
As mentioned, sterile packaging provides a barrier that protects medical devices from potential sources of contamination, including dust, moisture, and bacteria. Besides that, the packaging should maintain this protection during transport, storage, and until the point of use.
Extended Shelf Life
Sterile packaging can significantly extend the shelf life of medical devices. By creating a protective environment that minimizes the entry of contaminants, the packaging helps preserve the sterility of the devices for an extended period. This is particularly crucial for devices with longer expiration dates or those used in emergency situations, where immediate access to sterile devices is essential.
Properly packaged and sterilized devices can be safely stored for longer durations without compromising their sterility, ensuring their availability when needed and reducing wastage.
Types of Sterile Packaging
With the aim of maintaining sterility and protecting against contamination, different types of sterile packaging are utilized in the medical device industry. Each type serves a specific purpose in safeguarding the device and maintaining its functionality.
There are three main types of sterile packaging:
- Primary packaging: This is the packaging that is in direct contact with the medical device, and it’s typically made of materials that are impermeable to microorganisms, such as paper, plastic, or metal.
- Secondary packaging: Secondary surrounds the primary packaging, and it’s typically made of materials that are strong and durable, such as cardboard or plastic.
- Tertiary packaging: This packaging is used to transport and store medical devices, and it’s typically made of materials that are corrosion-resistant and protect the devices from damage, such as metal or plastic containers.
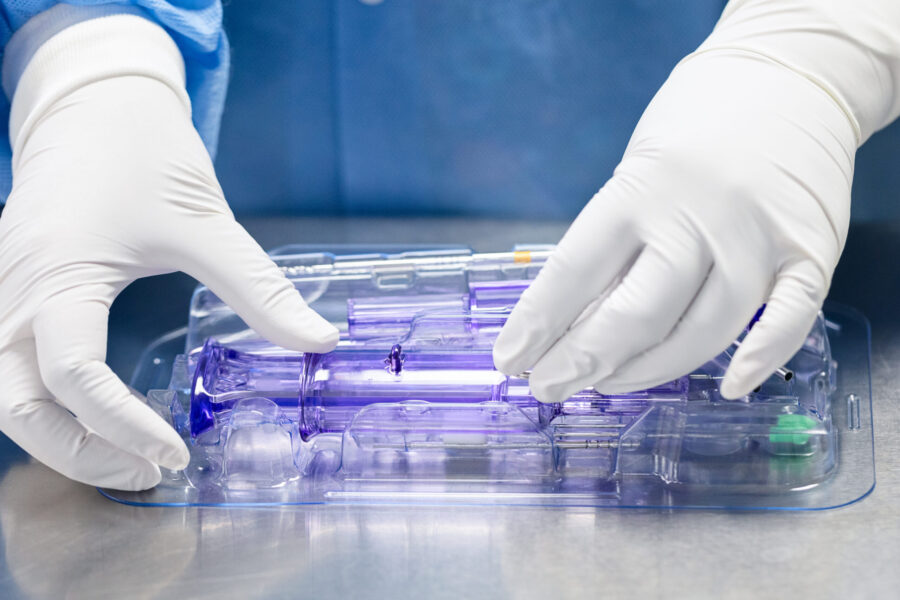
In addition to primary, secondary, and tertiary packaging, it’s worth mentioning peelable pouches and thermoform trays as popular types of sterile packaging. Peelable pouches are designed to maintain sterility and allow aseptic presentation, whereas thermoform trays are used to provide customized, secure positioning for devices in a sealed tray.
Materials Used in Sterile Packaging
Materials used in sterile packaging are another important factor to take into consideration since they need to fulfill specific requirements, including being compatible with the sterilization process, maintaining sterility, and providing adequate protection for medical devices. Some commonly used materials are:
- Paper: Medical-grade paper is often used for primary packaging, such as pouches or wraps. It is designed to be permeable to sterilizing agents while preventing the passage of microorganisms.
- Plastic: Various types of plastic, such as polyethylene, polypropylene, or polyvinyl chloride (PVC), are commonly employed in sterile packaging. Plastic materials offer excellent barrier properties, protecting devices from moisture, gasses, and contaminants. They are used for primary packaging, blister packs, trays, and clamshells.
- Cardboard: Cardboard or paperboard is often used for secondary packaging, such as cartons or boxes. It provides structural support, ensuring the integrity of the primary packaging and facilitating handling and transportation.
- Adhesive Tapes: Adhesive tapes play a vital role in securing sterile packaging. They are used to seal pouches or wraps, ensuring a tight closure and preventing the entry of contaminants.
The selection of the appropriate material should carefully consider different factors to ensure the sterility and integrity of medical devices throughout their lifecycle. The same applies to sterile packaging methods.

Sterile Packaging Methods
Once the appropriate materials for sterile packaging have been selected, it is crucial to employ suitable sterile packaging methods to achieve and maintain the desired level of sterility. Here are some that are commonly used:
- Heat Sealing: Heat sealing is used for creating a secure seal on pouches or wraps. It involves applying heat and pressure to melt the packaging material, resulting in a tightly sealed package that prevents the entry of contaminants.
- Induction Sealing: This method is commonly used for sealing containers with metal or aluminum foil seals. In this process, an induction sealing machine applies an electromagnetic field that generates heat in the foil, creating a hermetic seal on the container.
- Tyvek® Pouches: Tyvek® is a nonwoven material composed of high-density polyethylene fibers and it’s frequently utilized for the primary packaging of medical devices. It provides excellent microbial barrier properties while allowing the passage of sterilizing agents.
- Clamshell Packaging: This type of packaging consists of a hinged, transparent plastic container that securely encloses the medical device. It offers visibility and protection, allowing easy identification and access to the device while keeping it sterile.
- Tray and Lid Systems: Tray and lid systems are used for organizing and securing multiple medical devices within a sterilized tray. The tray and lid are typically made of durable materials, such as plastic or metal, providing protection during transportation and storage.
Sterilization Techniques
After the sterile packaging has been completed, the next crucial step is to apply effective sterilization techniques to ensure the elimination of microorganisms and maintain the sterility of the packaged medical devices.
The chosen sterilization technique will depend on various factors, including the type of medical device, its materials, packaging, regulatory requirements, and desired sterility assurance level. However, each of them offers its advantages, limitations, and suitability for specific devices and materials. These are the most common sterilization techniques
- Ethylene oxide gas: Ethylene oxide gas sterilization is commonly utilized due to its effectiveness against a broad spectrum of microorganisms. This low-temperature process offers excellent penetration, making it suitable for a wide range of materials. It is particularly advantageous for devices with complex geometries or those that cannot withstand high temperatures.
- Gamma radiation: Gamma radiation is a rapid and effective method that can penetrate various packaging materials, including plastic and paper. It damages the DNA of microorganisms, rendering them unable to reproduce. However, it is important to ensure that the appropriate dosage is used to achieve the desired level of sterilization without causing damage to the device.
- Steam sterilization: Steam sterilization, also known as autoclaving, is widely used for sterilizing heat-stable medical devices and materials. It involves exposing the device to high-pressure saturated steam at a specific temperature for a predetermined duration.
- Plasma sterilization: Plasma sterilization is a newer method that uses hydrogen peroxide plasma to sterilize in a low-temperature environment, making it suitable for heat-sensitive devices.
It is important to note that all methods must conform to the standards set by international standards organizations like ISO (International Organization for Standardization) and ASTM (American Society for Testing and Materials).

Packaging Validation and Why is it Important
What comes next is packaging validation. This critical process typically involves:
- Installation Qualification (IQ)
- Operational Qualification (OQ) and
- Performance Qualification (PQ).
Validation ensures that the packaging not only maintains sterility under expected conditions but also can withstand the physical stresses of distribution, handling, and storage, thereby ensuring the package’s integrity until it reaches the end-user. It’s also a crucial step in demonstrating that the packaging system is reliable and compliant with regulatory standards.
We talked about this process earlier, so check this link if you want to learn more about its components and challenges.
Quality Control in Sterile Packaging
Quality control is the final step in the sterile packaging process. It involves routine checks and inspections throughout the packaging and sterilization process. These checks ensure that every package that leaves the facility is safe, sterile, and ready for use. The most common methods of quality control include:
- Visual Inspection: This method involves examining the packaging for any physical defects, such as punctures, tears, or improper seals. It’s typically performed using specialized equipment and trained personnel to ensure accuracy.
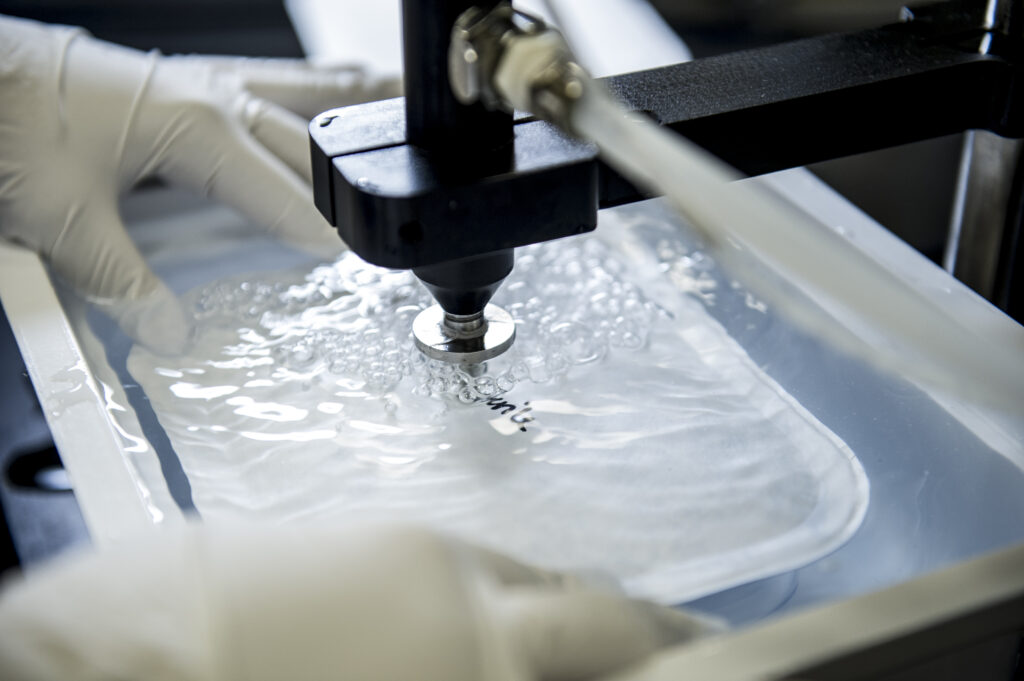
- Package Integrity Testing: Various methods can be employed to assess the integrity of the packaging, such as bubble emission testing, dye penetration testing, or vacuum decay testing. These tests determine if there are any leaks or breaches in the packaging that could compromise its sterility.
- Microbiological Testing: Microbiological testing involves taking samples from the packaged devices and testing them for the presence of microorganisms. It helps ensure that the sterilization process has effectively eliminated any potential contaminants. Examples include LAL and Bioburden testing.
- Accelerated Aging: Accelerated aging tests simulate the effects of time on the packaging by subjecting it to accelerated conditions such as high temperature and humidity. This helps assess the stability and performance of the packaging over its expected shelf life.
- Documentation and Record-Keeping: Proper documentation and record-keeping are crucial for quality control in sterile packaging. They serve as evidence of compliance with regulations and can be used for traceability and accountability purposes.
By implementing robust quality control measures, manufacturers can identify and rectify any issues with the packaging process, ensuring that every package meets the required standards of sterility and safety. This helps minimize the risk of infections or complications associated with contaminated medical devices and instills confidence in healthcare providers and patients regarding the reliability and effectiveness of packaged devices.
Conclusion
As you can see, sterile packaging for medical devices is a complex topic. It involves a combination of rigorous standards, advanced materials, and precise manufacturing techniques designed to protect patient safety, meet regulatory requirements, and ensure that devices remain sterile until used.
In this intricate landscape, the selection of a reliable and experienced packaging and assembly partner becomes vital to achieving these goals. A reputable contract packaging and assembly manufacturer brings expertise in navigating regulatory guidelines and ensuring compliance. Besides that, by choosing a reliable partner, manufacturers can focus on their core competencies while entrusting the task of sterile packaging to experts. In case you’re looking for one – you came to the right place. Reach out to us or drop us a comment if you have any questions or if you’d like more information on how packaging and assembly services can support your needs.
Summary:
- Sterile packaging for medical devices is essential for patient safety, regulatory compliance, and protection against contamination.
- There are various methods of packaging and sterilization, each designed to work together for greatest efficacy. .
- The selection of packaging and sterilization methods depends on the device’s characteristics and intended use.
- Packaging validation and quality control are critical processes that ensure the sterility and safety of packaged medical devices.
- Choosing a reliable and experienced packaging and assembly partner is crucial to ensure regulatory compliance.