The Medical Device Packaging Development Process
When it comes to successfully commercializing medical devices, the packaging process plays an incredibly important role. This process involves various steps, such as design and layout, materials selection, sterilization compatibility, validation testing like accelerated aging and vibration resistance, and compliance testing – all before production commences.
In this post, we’ll cover the different stages of developing safe, secure, and effective medical device packaging for your product. Read on to see what needs to be taken into consideration during every stage to reduce the risk of contamination or damage as your product moves through distribution channels.
Understanding the Medical Device Packaging Development Process
Before we can get into the specifics of medical device packaging development, it is important to understand how the entire process works. Medical device packaging and assembly involves a number of interrelated steps, from concept through production.
The goal of the process is to ensure that the appropriate packaging is used to protect a sterile medical device all the way through storage and distribution until it reaches the end patient. The particular phases of the process can vary depending on the complexity and purpose of the device itself. Yet, most will go through six distinct stages:
- Understand and Clarify Customer Requirements
- Packaging Design & Development
- Material Selection
- Validation Testing
- Sterilization
- Production & Label Design
Clarify customer requirements
The packaging development process begins with understanding the customer’s requirements. This critical step sets the tone for the rest of the process and is an important opportunity to clarify the type of device, size, weight, and materials used. It is also important to determine the sterilization requirements because those can impact the type of packaging we recommend.
Also, we need to determine if the device is a candidate for pre-validated packaging, which can save the customer time and money.
We pride ourselves on listening closely to the customer at this stage and clarifying the critical details early on so that we can design a packaging and assembly protocol that is most appropriate for that customer’s specific needs.
These early conversations also guide choices related to the sterilization method and requirements. For example, packaging for terminally sterilized medical devices must follow ISO 11607 standards. These standards guide the level of sterilization, the sterilization method, and the type of packaging material that should be used.
Ultimately, all of these elements need to be considered to determine the most suitable packaging for the medical device.
The factors to consider include:
- Device Dimensions, Weight, Density, and materials used
- Sterilization Compatibility and Requirements
- Packaging Material Needs
- Validation Testing – accelerating aging and distribution testing
- Regulatory Requirements
In order to address these factors, you and your contract packaging partners should answer the following questions:
- How will the device be used?
- What materials are compatible with its purpose?
- How will the device be affected by temperature and moisture?
- What type of package will best protect and secure the product?
- Does it need a combination of materials for multiple layers of protection?
- What kind of environment will the device be stored and used in?
- What are the sterilization requirements for your device?
- Are there any special regulatory requirements?
Once these considerations have been taken into account, the packaging design process begins. Depending on the complexity of the device and its components, this can include different materials selection, layout, and testing. But let’s start by looking at the process itself.
Packaging Design & Development

When it comes to the actual design of the package, every detail counts. The package should be functional and durable as well as cost effective. Most importantly, it should protect the device and keep it sterile during all stages of the distribution channel and while in storage. It needs to be protected all the way to its intended use for the end patient.
When designing the package, it’s important to consider all of the elements that will impact its performance, such as:
- Package material and design
- Medical device weight and dimensions
- Seals and labels
- Sterilization method
- Shipping and storage requirements
- Cost
This is also the stage where the engineers and sales people work with the customer to determine whether the device is a candidate for pre-validated packaging. A pre-validated package has already been tested and approved for use, and eliminates the need to conduct stability testing and seal-strength validation tests. If the device meets these requirements, it can save the customer a significant amount of time and money. If not, then the contract manufacturer will explore custom-designed packaging options.
Cost is obviously a significant consideration as well. It takes an expert who understands the regulations and knows what works in practice from years of experience so that the packaging isn’t “overbuilt”. Adding extra packaging may work in the short term to protect the device, but wouldn’t be cost effective, and therefore, not viable.
Finally, the package should also contain labeling and instructions for use in order to meet regulatory requirements, which can include information such as bar codes and expiration dates. Location and visibility for labels is an important part of the label design process to ensure trackability during production, shipping and sterilization.
Material Selection
The type of material you choose for your device’s packaging is just as important as the design itself, and goes hand in hand with the design process. Different materials provide different levels of protection, so it’s important to select one that is compatible with the device and its intended use. Consideration also has to be given to the sterilization method planned, because different packaging material choices work better for each sterilization method.
Common materials used in packaging design include:
- Thermoformed Plastic, such as Polyethylene and PVC
- Paperboard/Vinyl composites
- Polypropylene Films
- Foam Inserts and more.
These materials can be used alone or in combination with others to provide multiple layers of protection. For example, you may choose to use a paperboard sleeve with a foam insert for shock absorption and an inner plastic bag for added moisture protection.
The type of package design that you select will also depend on your needs and budget, as well as the complexity of the device.
Here is a great in-depth article about selecting materials for medical products if you’d like to know more about this part of the process.
Validation Testing
At this stage, various validation tests are performed to ensure that the packaging meets protection and safety requirements for medical devices. These typically focus on accelerated aging of the package and product to see how it holds up over time at different temperatures. Distribution testing is also done to determine the stability and durability of the packaging to withstand simulated shipping conditions. The package needs to be able to withstand various environmental conditions during its journey from the medical device manufacturer’s facility to its end-user location – the patient.
ISO and ASTM standards are used as benchmarks to make certain that the proper qualifications are met. ISO 11607 provides guidance specifically for validating terminally sterilized medical device packaging in these key areas:
- Performance/Dynamics Testing
- Stability Testing (accelerated and real-time aging)
- Distribution Simulation
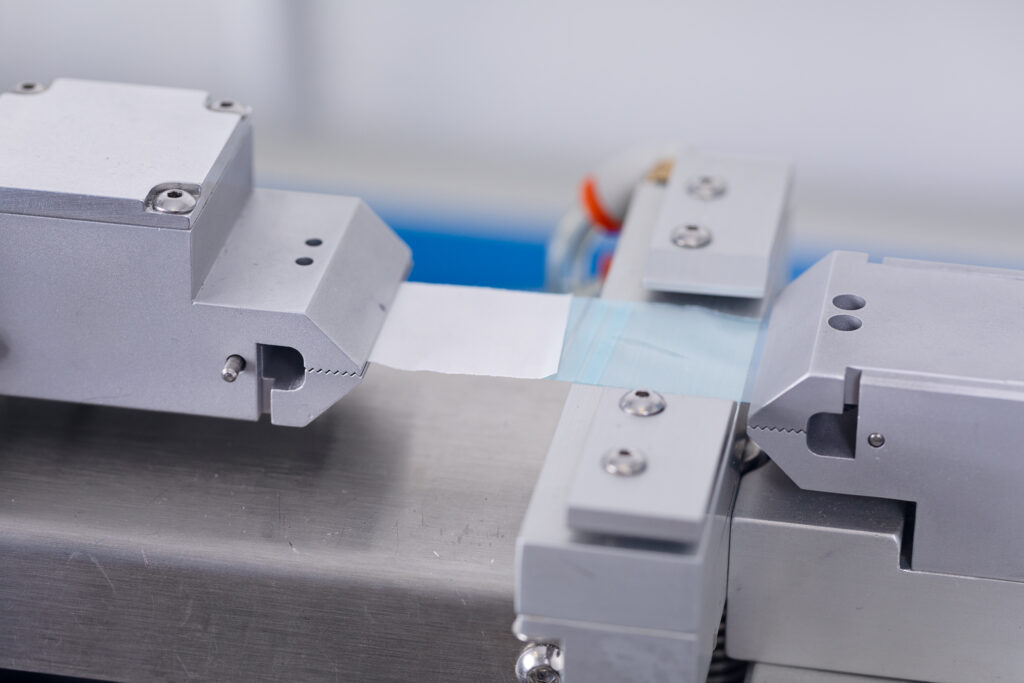
- Package Seal Strength Testing
- Package Integrity Testing
This is why pre-validated packaging, which has already met these validation testing requirements, can be so useful in saving medical device customers time and money.
Sterilization

Now that the materials have been selected, it’s time to decide on the type of sterilization that will be used. The three most common sterilization methods are:
- Ethylene Oxide (ETO)
- Gamma Radiation
- Steam
This is an important step since, as we mentioned previously, the type of sterilization used for the medical device will also affect the packaging choice itself.
For example, if the device requires steam sterilization, then the container must be able to withstand high temperatures and moisture levels. Alternatively, if it requires irradiation or ethylene oxide (ETO) sterilization, a different material may be needed that is compatible with these sterilization methods.
Additionally, most sterilization is performed by specialized third parties, and it is difficult to break into their cue if the contract packaging company does not already have an established relationship.
Production & Labeling
 Now you are ready to begin production. As part of the preceding steps, there should have been discussions to plan whether assembly and packaging needs to be conducted in a cleanroom environment and to what standard. Most medical devices require ISO Class 7 or Class 8 cleanroom environments, which refers to the number of particles per square foot of air. This is governed by ISO standard 14644-1.
Now you are ready to begin production. As part of the preceding steps, there should have been discussions to plan whether assembly and packaging needs to be conducted in a cleanroom environment and to what standard. Most medical devices require ISO Class 7 or Class 8 cleanroom environments, which refers to the number of particles per square foot of air. This is governed by ISO standard 14644-1.
Pre-assembly tests should be run to determine the optimal assembly method and equipment layout to make production as efficient as possible and minimize costs. Quality considerations are also important to ensure that the process promotes adherence to established quality standards and production checks are placed at key points along the way to monitor the process. Assemblers should be trained on the optimal process and empowered to suggest improvements along the way.
Labeling is another key part of the production process. Labels need to be designed earlier on; in fact, the earlier label decisions are made, the better, to ensure that they work together with the packaging design. During the production phase, it is important to monitor that the appropriate labels are consistently applied to the correct inner and outer package and that a traceable bar code is visible at all times for real-time tracking. Label mistakes are one of the most common areas for quality missteps, so it is important to consider this key step as an integral part of the production process. It should be embedded in the quality process, and it is important to work with experienced contract manufacturers who have a robust and tested label quality control system in place.
Conclusion
Medical device packaging development is a complex process, and it shouldn’t be taken lightly as it requires a lot of planning, testing, and collaboration between the customer and contract manufacturer. However, by understanding the steps involved and taking the time to properly design and validate the packaging, you can be sure that your device will reach its end destination safely and securely.
It’s also true that each medical device project has a unique process, so there may be some variation in the order or length of time spent in each phase depending on your product.
Besides all the steps involved, having a team of skilled and experienced professionals, as we do here, at PRO-TECH Design, is key to success. The right team can make all the difference in ensuring that your medical device packaging is of top quality and meets all regulatory requirements.
FAQ
What are the FDA requirements for medical device packaging?
The U.S. Food and Drug Administration (FDA) regulates the design, manufacture, and distribution of medical devices through its Medical Device Quality System Regulation (QSR).
The QSR requires that all medical devices be packaged in accordance with safety standards, as well as providing adequate product protection from environmental hazards such as oxygen, moisture, and light. In addition, medical device packaging must be labeled properly in order to comply with FDA regulations.
What are the ISTA standards for medical packaging?
The International Safe Transit Association (ISTA) provides performance standards for testing the durability and protection of medical device packaging.
These standards include tests for shock, vibration, temperature, pressure, and humidity in order to simulate real-world conditions. The testing is designed to verify that the package can withstand a range of conditions without compromising its effectiveness in protecting the medical device.
What is ISO 11607?
ISO 11607 is an international standard that outlines the requirements for medical device packaging. The standard covers the design, development, testing and validation of packages used to contain and transport sterile medical devices. It also specifies labeling requirements in order to ensure that sterile products are correctly identified.
What types of sterilization are available?
The most common type of sterilization used for medical devices is ethylene oxide sterilization. This process utilizes gas to kill bacteria, viruses, and other microorganisms on the device in order to render it sterile.
Other types of sterilization include gamma radiation and steam. It’s important to note that the type of sterilization selected will depend on the type of medical device and its intended use.
What if I switch to another sterilization method?
Sometimes, a company will choose one method of sterilization only to realize that another method is more suitable for their needs. In this case, they may need to redesign the package in order to ensure it meets all of the requirements for the new sterilization method.
In some cases, it’s possible to switch between sterilization methods without having to redesign the package. However, it’s best to consult with your contract manufacturer or packaging expert if you plan on making any changes.
What Is Human Factors Engineering?
Human Factors Engineering (HFE) is an important part of the medical device packaging development process. HFE focuses on making sure that a package is designed and tested to ensure it meets the needs of intended users. This includes considering factors like ergonomics, usability, and user interfaces in order to create packages that are safe, effective, and easy to use.
What are the usability concerns?
When designing medical device packaging, it’s important to consider usability. Usability refers to the ease with which a user can interact with and open the package as well as understand any instructions included in the package. This is especially true for packages designed for use by patients who may not have a lot of experience opening or understanding complex packages.
To ensure usability, consider the approximate size and shape of the package as well as any instructions that may be included.
What are the validation criteria for medical packaging?
The validation criteria for medical device packaging are outlined in ISO 11607 we already mentioned. The standard requires that packages be tested to ensure they meet certain performance requirements and provide adequate protection for the product throughout its lifecycle. In addition, the package should be labeled in accordance with FDA regulations and must clearly identify the product and its contents.
What are the compatibility issues with ethylene oxide?
When using ethylene oxide as a sterilization method, it’s important to consider any compatibility issues that may arise.
Certain materials used for packaging can be negatively affected by ethylene oxide and may need to be replaced with materials that are more compatible with the sterilant. It’s also important to keep in mind that certain components within the package may not be compatible with the sterilization process, so they should be avoided or replaced if necessary.
What is Final Seal Testing?
Final seal testing is the last step in the medical device packaging development process. This type of testing ensures that a package has been properly sealed and can withstand any environmental changes it may encounter throughout its lifecycle.
It’s important to note that this type of testing must be performed by an accredited laboratory in order for a package to meet FDA standards.

